Sarah Martinez remembers the exact moment her world shifted. Sitting in her doctor’s office last spring, she heard the words “your cancer is back” for the second time in three years. The tumor had returned, smaller this time, but somehow more frustrating. “It’s like playing hide and seek with something that knows all your moves,” she told her sister that night.

What Sarah didn’t know was that researchers across the country were working on a solution to exactly this problem. They weren’t just trying to kill cancer cells faster or harder. They were figuring out how to make them impossible to hide.
The breakthrough sounds almost too simple: if cancer cells are master disguise artists, why not force them to wear bright, unmistakable costumes that scream “attack me” to every immune cell in the area?

Making the invisible enemy show its face
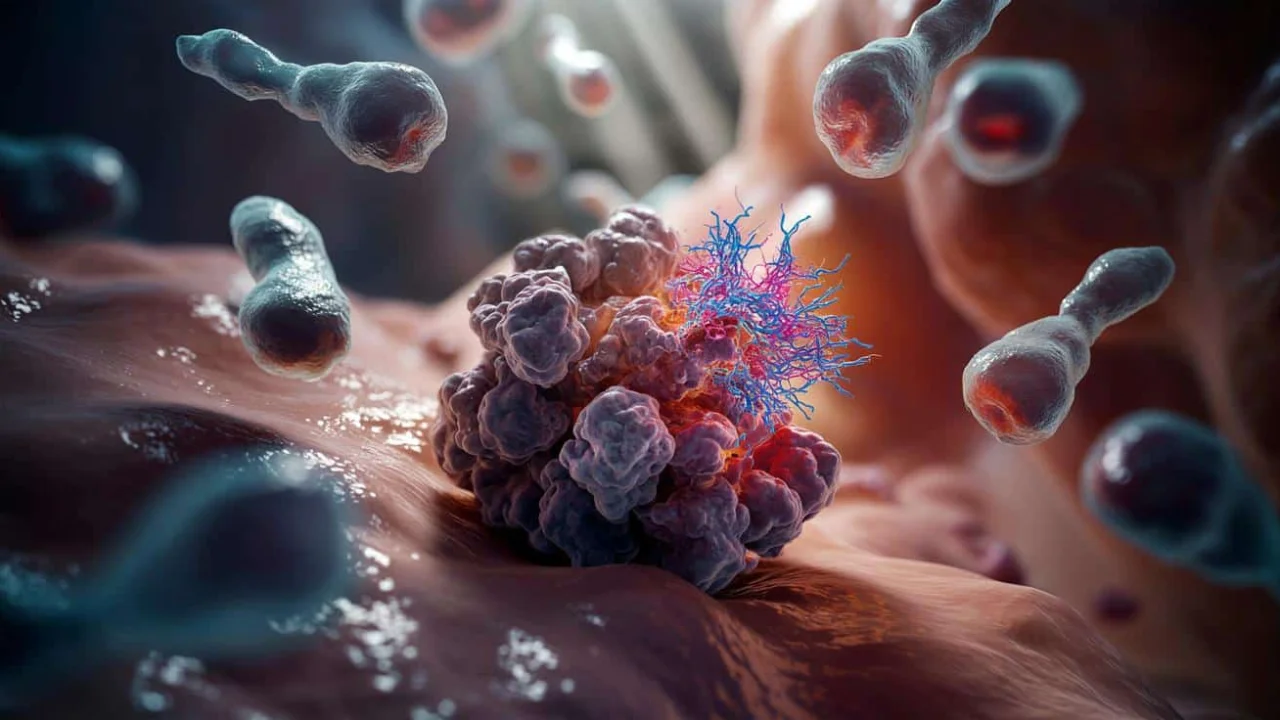
This new cancer immunotherapy strategy works like installing floodlights in a dark alley where criminals used to hide. Scientists have developed techniques that essentially “tag” cancer cells with proteins that act as giant neon signs for the immune system.
The approach targets one of cancer’s sneakiest survival tricks. Normal cells display bits of their internal proteins on their surface, like showing an ID card to passing immune cells. Healthy cells show normal IDs. Infected or damaged cells display abnormal proteins that trigger immune attacks.

“Cancer cells have learned to either hide their abnormal proteins or display fake normal ones,” explains Dr. James Chen, an immunologist at Stanford University. “We’re essentially forcing them to show their true colors.”
The strategy involves several cutting-edge techniques working together. Some treatments use engineered viruses that specifically infect cancer cells and force them to produce highly visible target proteins. Others use small molecules that block the cellular machinery cancer uses to hide its abnormal proteins.

Think of it like removing someone’s disguise and then painting them bright orange. Once tagged, cancer cells become sitting ducks for T-cells, natural killer cells, and other immune warriors that were previously fooled by the disguise.
The science behind turning cancer cells into targets
The technical details reveal just how sophisticated this cancer immunotherapy strategy has become. Researchers are using multiple approaches to ensure cancer cells can’t slip back into hiding.

- Viral vectors: Modified viruses that only infect cancer cells, forcing them to produce immune-activating proteins
- Checkpoint inhibitor combinations: Drugs that remove the “don’t attack” signals cancer cells use to protect themselves
- Synthetic biology: Engineered immune cells programmed to recognize specific cancer markers
- Epigenetic modifiers: Treatments that change how genes are expressed in cancer cells, revealing hidden targets
- Monoclonal antibodies: Lab-made proteins that stick to cancer cells like molecular Post-it notes
Early clinical trials show promising results across different cancer types. The visibility strategy appears especially effective against cancers that traditionally hide well, including certain brain tumors and metastatic melanomas.
| Cancer Type | Traditional Response Rate | With Visibility Strategy | Trial Stage |
|---|---|---|---|
| Glioblastoma | 15-20% | 45-50% | Phase II |
| Metastatic Melanoma | 25-30% | 65-70% | Phase III |
| Pancreatic Cancer | 5-10% | 25-30% | Phase I |
| Triple-Negative Breast | 20-25% | 55-60% | Phase II |
“The numbers are encouraging, but what excites me most is how durable the responses appear to be,” notes Dr. Maria Rodriguez, lead researcher on several visibility trials. “When the immune system learns to see cancer clearly, it seems to remember that lesson.”
What this means for patients and families
For people like Sarah Martinez, this cancer immunotherapy strategy represents hope in a very practical form. Instead of treatments that work for a few months before cancer adapts, the visibility approach creates lasting immune memory.
The treatment process itself varies depending on the specific approach used. Some patients receive engineered viruses through direct injection into tumors. Others get intravenous infusions of modified immune cells or targeting antibodies.
Side effects tend to be different from traditional chemotherapy. Instead of general toxicity, patients might experience immune-related effects as their newly activated immune systems learn to attack cancer more aggressively.
“We’re seeing fatigue and some autoimmune-like symptoms, but they’re generally manageable and temporary,” explains Dr. Chen. “The trade-off is often worth it when you consider the alternative.”
The psychological impact cannot be understated. Patients who have lived with the fear of invisible, undetectable cancer recurrence are finding comfort in treatments that make cancer cells essentially announce themselves.
Cost and accessibility remain significant hurdles. These personalized treatments require sophisticated manufacturing and delivery systems. However, several pharmaceutical companies are investing heavily in scaling production.
For oncologists, the strategy represents a fundamental shift in thinking. Instead of just poisoning cancer cells or blocking their growth, they’re now recruiting the patient’s own immune system as a permanent surveillance force.
The visibility approach also works well in combination with existing treatments. Radiation therapy, for example, can damage cancer cells in ways that make the visibility strategy even more effective.
Looking ahead, researchers are exploring whether the strategy could work as a preventive measure for people at high cancer risk. The idea of training immune systems to recognize and eliminate early cancer cells before they become tumors is tantalizing.
Sarah Martinez recently started a visibility-based treatment at her cancer center. Three months in, her latest scan showed no detectable cancer. More importantly, her immune cells show strong activation against cancer markers.
“For the first time in years, I feel like my body is working with the treatment instead of just enduring it,” she says. “That changes everything about how you face each day.”
FAQs
How long does it take for this cancer immunotherapy strategy to work?
Most patients see initial immune activation within 2-4 weeks, with measurable tumor response typically occurring within 8-12 weeks of starting treatment.
Does this approach work for all types of cancer?
The strategy is most effective against cancers that traditionally hide from the immune system, though researchers are testing it across many cancer types with varying degrees of success.
Are the side effects similar to chemotherapy?
No, side effects are usually immune-related rather than toxic, including fatigue, skin reactions, and occasional autoimmune symptoms that are generally manageable.
Can this treatment be combined with other cancer therapies?
Yes, the visibility strategy often works well alongside radiation, surgery, and even some chemotherapy drugs, potentially making them more effective.
How much does this cancer immunotherapy strategy cost?
Current treatments range from $50,000 to $200,000 per course, though costs are expected to decrease as production scales up and more competitors enter the market.
Will insurance cover these new treatments?
Coverage varies by insurance provider and specific treatment, but many are beginning to cover visibility-based therapies as clinical trial data demonstrates their effectiveness.