
Sarah stared at the lab results spread across her kitchen table, the words blurring together through her tears. Stage 3 breast cancer. The phrase felt foreign, like it belonged to someone else’s story. Her 8-year-old daughter Emma was upstairs doing homework, completely unaware that their world had just shifted.
Three months later, Sarah sat in a different chair, this time in a research hospital. The oncologist pulled up two scans on his computer screen. “This is your tumor from last month,” he said, pointing to a shadowy mass that looked deceptively quiet. “And this,” he clicked to the next image, “is after the new treatment. See how it’s lighting up?”
The difference was startling. Where before there had been vague, ghostly shapes, now there were bright, clearly defined targets. “Your immune system can finally see what it’s fighting,” he explained. For the first time since her diagnosis, Sarah felt something she hadn’t dared to feel: hope.

The invisibility cloak that cancer wears
Cancer has always been a master of disguise. These rogue cells don’t announce themselves with flashing neon signs. Instead, they slip past our body’s security system by mimicking normal, healthy tissue. Think of them as sophisticated imposters wearing perfect ID badges.
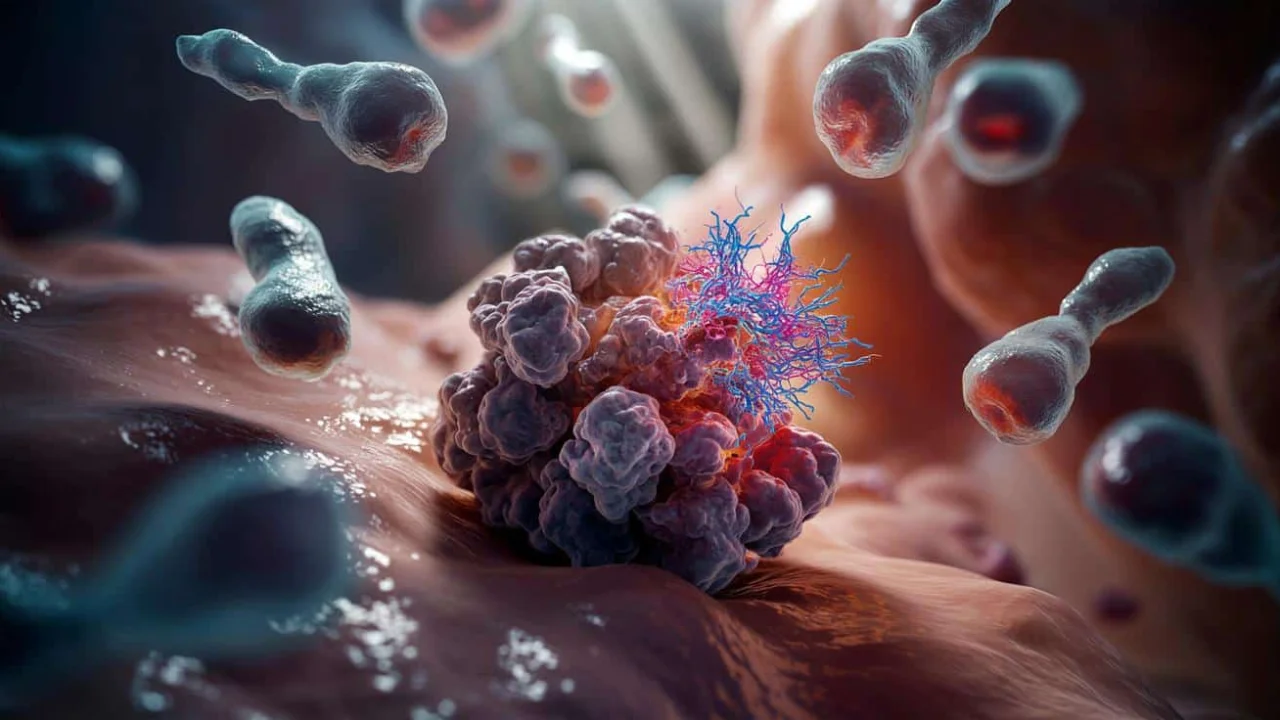
Our immune system works like a highly trained security force, constantly patrolling for threats. But when cancer cells become invisible to these defenders, they can grow and spread unchecked. The new breakthrough focuses on stripping away this invisibility cloak, making cancer cells visible to immune detection.

“We’re essentially teaching the immune system to recognize what it should have been fighting all along,” explains Dr. Maria Rodriguez, a leading immunotherapy researcher. “It’s like giving someone glasses for the first time – suddenly they can see clearly what was always there.”
The strategy works by targeting specific proteins that cancer cells use to hide. When these proteins are blocked or modified, the cancer cells suddenly become visible to passing immune cells. It’s a simple concept with profound implications.

How scientists are lighting up the enemy
The technical details behind making cancer cells visible involve several cutting-edge approaches. Researchers are testing multiple methods simultaneously, each targeting different aspects of cancer’s camouflage system.
Here are the main strategies currently showing promise:

- Checkpoint inhibitor enhancement: Blocking proteins that normally tell immune cells to “stand down”
- Antigen presentation boosting: Helping cancer cells display more danger signals on their surface
- Metabolic targeting: Disrupting the energy systems that cancer cells use to stay hidden
- Biomarker amplification: Making existing cancer markers more visible to detection systems
- Combination therapy approaches: Using multiple visibility techniques together for maximum effect
The most promising results come from combining these approaches. Early trials show that when cancer cells become fully visible, immune response rates jump dramatically.
| Treatment Approach | Visibility Increase | Immune Response Rate | Trial Phase |
|---|---|---|---|
| Single checkpoint inhibitor | 30-40% | 25% | Phase III |
| Combination therapy | 70-85% | 58% | Phase II |
| Enhanced antigen display | 60-75% | 45% | Phase II |
| Metabolic disruption | 45-55% | 35% | Phase I |
“The numbers speak for themselves,” notes Dr. James Chen, who leads clinical trials at a major cancer center. “When we can make cancer cells truly visible, the immune system does what it was designed to do – it fights back effectively.”
What makes this approach particularly exciting is its precision. Unlike traditional chemotherapy, which affects both healthy and cancerous cells, visibility enhancement specifically targets the mechanisms cancer uses to hide.
What this means for patients and families
The real-world impact of making cancer cells visible extends far beyond laboratory results. For millions of patients worldwide, this could represent a fundamental shift in how cancer is treated.
Traditional treatments often feel like fighting an enemy in the dark. Chemotherapy and radiation work by attacking rapidly dividing cells, but they can’t distinguish between cancer and healthy tissue. This new approach is different – it’s about giving your own immune system the tools to win the fight.
Patients in early trials report fewer severe side effects compared to traditional chemotherapy. That’s because their own immune systems are doing the heavy lifting, rather than toxic drugs.
“My energy levels stayed much higher during treatment,” shares Maria Santos, a trial participant. “I could still take my kids to school, still work part-time. The treatment worked with my body instead of against it.”
The approach also shows promise for cancers that have traditionally been difficult to treat. Pancreatic cancer, brain tumors, and certain blood cancers – all notorious for their ability to evade detection – are responding to visibility enhancement strategies.
For healthcare systems, the implications are equally significant. Treatments that harness the patient’s own immune system could prove more cost-effective than current standard therapies, while potentially offering better outcomes.
However, challenges remain. Not all patients respond equally well to immune-based treatments. Researchers are working to identify which patients will benefit most from making their cancer cells visible, and how to optimize the approach for different cancer types.
Dr. Rodriguez emphasizes the broader significance: “We’re not just treating cancer differently – we’re changing how we think about the relationship between cancer and the immune system. This visibility approach could be the foundation for preventing cancer recurrence in ways we’ve never been able to before.”
The timeline for widespread availability varies by cancer type and treatment combination. Some approaches are already in late-stage trials, while others are still being refined in earlier phases. But for patients and families facing cancer today, the progress represents genuine reason for optimism.
As research continues, the focus remains on making these visibility-enhancing treatments as effective and accessible as possible. The goal isn’t just to treat cancer – it’s to give every patient’s immune system the best possible chance to win the fight.
FAQs
How exactly do scientists make cancer cells visible to the immune system?
They use various techniques to remove or block the proteins cancer cells use to hide, essentially stripping away their camouflage so immune cells can recognize them as threats.
Is this treatment approach available to patients now?
Some versions are available through clinical trials, while others are still in development. The availability depends on the specific cancer type and treatment combination.
What are the side effects compared to traditional chemotherapy?
Early trials suggest fewer severe side effects since the treatment works with the immune system rather than using toxic drugs that affect all rapidly dividing cells.
Can this approach work for all types of cancer?
Research shows promise across many cancer types, but effectiveness varies. Scientists are working to identify which patients and cancer types respond best to visibility enhancement strategies.
How long before this becomes standard cancer treatment?
The timeline varies by specific approach and cancer type. Some treatments are already in late-stage trials, while others need more research before widespread use.
Can this prevent cancer from coming back?
Early research suggests that training the immune system to recognize cancer cells could help prevent recurrence, but more long-term studies are needed to confirm this benefit.