
Sarah had watched her brother struggle for over two decades. Every family dinner came with the same careful dance—avoiding topics that might trigger his darkness, pretending not to notice when he disappeared mid-conversation into that familiar fog. When he called her last month, laughing at something silly on the radio, she almost didn’t recognize his voice.

“I forgot what this felt like,” he told her. After 31 years of treatment-resistant depression, her brother had found something that finally worked. Not another pill or therapy session, but a breakthrough that’s changing how we think about the most stubborn cases of depression.
For millions of people like Sarah’s brother, traditional treatments simply don’t work. They’ve tried everything—multiple antidepressants, therapy, even electroconvulsive treatments—only to remain trapped in a cycle that feels impossible to break.

When Nothing Else Works: The Reality of Treatment-Resistant Depression
Treatment-resistant depression affects roughly one-third of people diagnosed with major depression. That’s not a small number—we’re talking about millions of individuals who’ve watched friends and family members recover with standard treatments while they remain stuck.
“These patients often feel like failures, but they’re not,” explains Dr. Jennifer Martinez, a psychiatrist specializing in complex mood disorders. “Their brains are wired differently, and we’re finally developing tools sophisticated enough to address those differences.”

The condition is officially defined as depression that doesn’t respond to at least two different antidepressant medications tried for adequate periods. But that clinical definition barely captures the human reality—years of hoping each new treatment will be “the one,” followed by the crushing disappointment when symptoms persist.
Marc’s story from Zurich illustrates this perfectly. Starting antidepressants at 13, he spent three decades cycling through treatments. Twenty different medication regimens. Electroconvulsive therapy. Transcranial magnetic stimulation. Even experimental ketamine sessions. Each promised hope. None delivered lasting relief.
The Science Behind the Breakthrough
The game-changer for Marc—and potentially thousands of others—is personalized deep brain stimulation (DBS). This isn’t the crude, one-size-fits-all brain stimulation of the past. This is precision medicine applied to the mind.
Here’s how the new approach works compared to traditional treatments:

| Treatment Approach | How It Works | Success Rate | Timeline |
|---|---|---|---|
| Standard Antidepressants | Chemical flooding of brain | 60-70% initial response | 6-8 weeks |
| Traditional DBS | Generic brain stimulation | 40-50% in severe cases | 3-6 months |
| Personalized DBS | Custom circuit targeting | 70-80% in trials | 2-4 weeks |
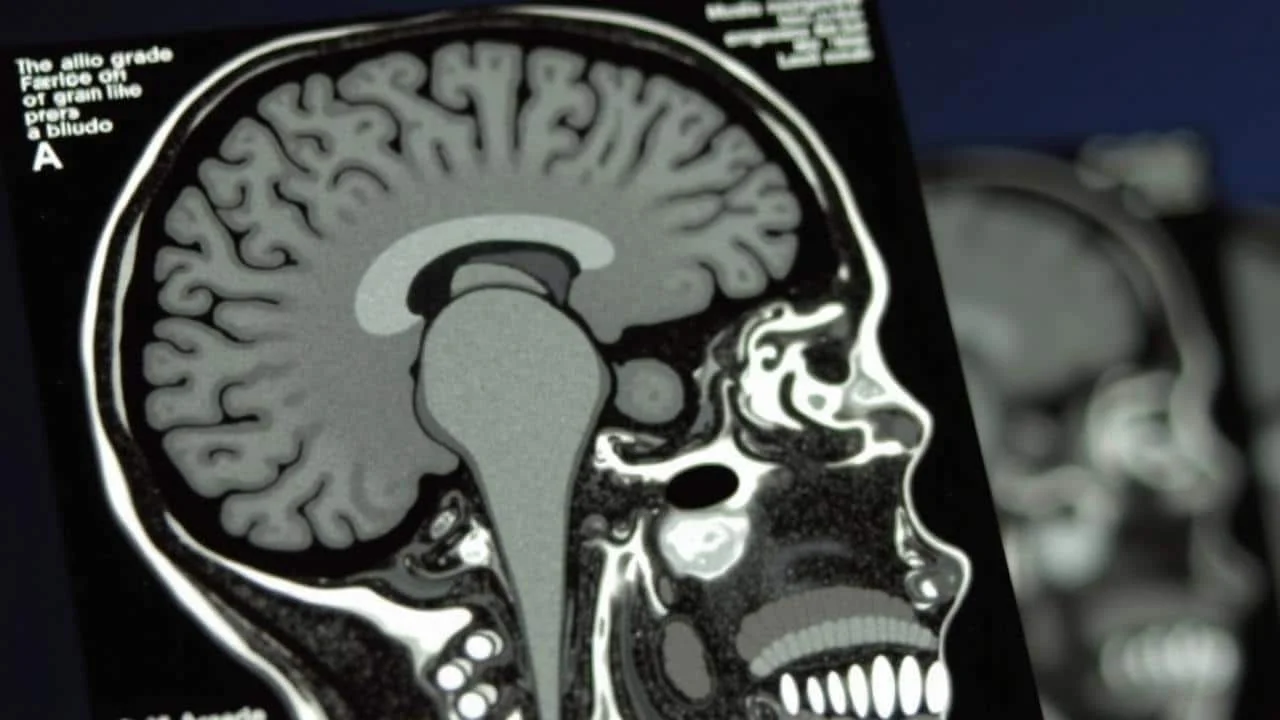
The personalized approach starts with weeks of brain mapping. Researchers use advanced MRI and functional imaging to identify each patient’s unique depression circuits. They’re literally looking at where sadness lives in the brain and how it connects to other regions.
“We’re not just asking how depressed someone feels anymore,” says Dr. Robert Chen, a neuroscientist involved in DBS research. “We’re trying to see depression physically, to trace it like a road map through the brain.”
Key features of the new personalized DBS include:
- Individual brain circuit mapping before any surgery
- Custom electrode placement based on personal brain anatomy
- Adjustable stimulation patterns that can be fine-tuned over time
- Real-time monitoring of brain activity and mood changes
- Integration with smartphone apps for continuous data collection
The surgery itself involves implanting thin electrodes in specific brain regions identified during the mapping process. Unlike traditional DBS that targets standard locations, these placements are as unique as fingerprints.
Who Could Benefit and What’s Coming Next
The most immediate candidates for personalized DBS are people who’ve exhausted conventional options. We’re talking about individuals who’ve tried multiple medications, various forms of therapy, and possibly other brain stimulation techniques without lasting success.
“This isn’t a first-line treatment,” emphasizes Dr. Martinez. “But for people who’ve been treatment-resistant for years, it represents genuine hope where there wasn’t any before.”
Current eligibility criteria typically include:
- Severe depression for at least two years
- Failure of at least four different antidepressant trials
- Significant impairment in daily functioning
- No active substance abuse or certain medical conditions
- Willingness to participate in long-term follow-up studies
The research is expanding rapidly. Teams in the US, Canada, and Europe are running parallel trials, each refining the technology and techniques. Early results suggest that about 70-80% of patients experience significant improvement within weeks of activation.
But perhaps more importantly, the effects seem to be lasting. Marc, now several months post-procedure, describes his recovery as “like someone turned the lights back on in my brain.” He’s returned to work, reconnected with old friends, and started planning for a future he couldn’t imagine six months ago.
“The most remarkable thing isn’t just that patients feel better,” notes Dr. Chen. “It’s that they feel like themselves again. They remember who they were before depression took over.”
The technology is still expensive and requires specialized medical centers. But as techniques improve and costs decrease, personalized DBS could become available to a much broader population within the next decade.
For families like Sarah’s, watching a loved one struggle with treatment-resistant depression, these advances offer something they hadn’t dared to hope for: the possibility that even the most stubborn depression might not be permanent after all.
FAQs
What exactly is treatment-resistant depression?
It’s depression that doesn’t improve after trying at least two different antidepressant medications for adequate periods, typically affecting about one-third of people with major depression.
How is personalized DBS different from regular brain stimulation?
Unlike standard approaches that target the same brain areas in everyone, personalized DBS maps each patient’s unique brain circuits first, then customizes electrode placement and stimulation patterns specifically for that person.
Who is eligible for this treatment?
Currently, candidates must have severe, long-term depression that hasn’t responded to multiple treatments, including at least four different antidepressants and other therapies.
How long does it take to see results?
Most patients in trials experience significant improvement within 2-4 weeks of activating the device, much faster than traditional treatments.
Is the surgery risky?
Like any brain surgery, there are risks, but the procedures are minimally invasive and performed by specialized neurosurgical teams with extensive experience in DBS techniques.
When will this be widely available?
While still in clinical trials, researchers expect the technology could become more broadly accessible within the next 5-10 years as techniques improve and costs decrease.